Home > Employee Benefits > Prescription Drugs
Prescription Drugs
The administration of the prescription drug program is processed through Anthem/CarelonRX. Please note that CarelonRx, the pharmacy division of Anthem, is referenced alongside Anthem.
To meet its fiduciary responsibility to the Health Plan, the Archdiocese of Cincinnati (AOC) benefits department issued a Request for Proposal (RFP) to potential pharmacy program administrators. Following a thorough review, it was determined that Anthem/CarelonRX is the best choice to manage our pharmacy benefit, offering the most cost-effective and clinically beneficial options, along with the best outcomes for members.
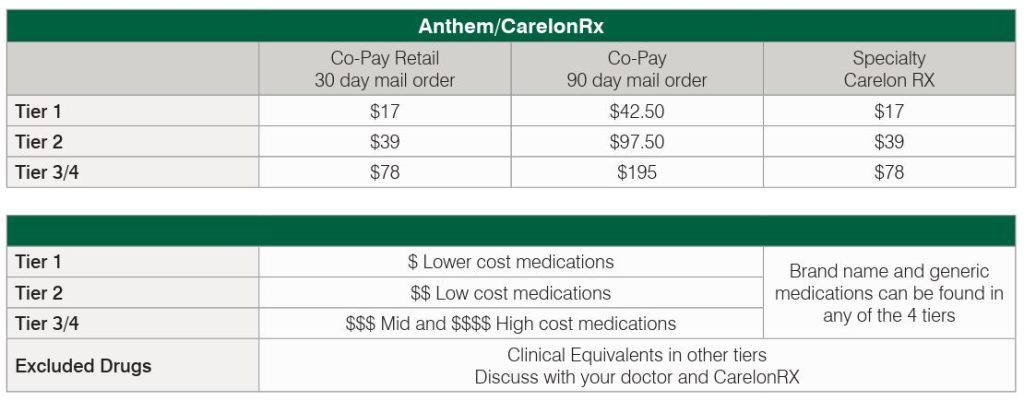
The benefit and copay structure of the pharmacy plan remains unchanged. However, there are adjustments to the list of covered drugs which may move some medications to a different tier. For a majority of members this results in a lower copay.
Major regional retail pharmacies used by our members are a part of the Anthem/CarelonRX network so you can continue to go to the pharmacy of your choice. Members taking specialty medications transition to Anthem’s Specialty Pharmacy, BioPlus, and members using Home Delivery have access to CarelonRx home delivery.
Key information:
- You will be able to access both your medical and pharmacy benefit information on the same platform via Anthem.com or the FREE Sidney Mobile App on digital device.
- Your medical and pharmacy benefit are combined into one ID card under Anthem.
- All enrolled members received a new ID prior to July 1, 2025.
Click here for the Anthem/CarelonRx Q&A
Creditable Coverage
The Archdiocese of Cincinnati Health Plan has determined that the prescription drug coverage offered by Anthem/CarelonRx is, on average for all plan participants, expected to pay out as much as standard Medicare prescription drug coverage pays and therefore considered Creditable Coverage.
Download the Certificate of Creditable Coverage for Prescription Drug Notice.
Lost ID Card
If you lose your Anthem/CarelonRx ID card, you can acquire a new one by one of the following options:
- Call Anthem Customer Service at 1.833.727.2165
- Register at Anthem.com – download/print or request copy to be mailed
- Download the Anthem Sydney App – have a digital ID card on mobile device
Prior Authorization
Your prescription drug plan requires prior authorization on certain medications. Prior authorization helps ensure select medications are prescribed according to FDA guidelines. If you are prescribed one of the medications that require prior authorization, you will be notified after you fill your first prescription. At that time, if you wish to keep using your medication, it must be pre-approved before your benefit plan will continue to cover it.
Your doctor can start the prior authorization review process by contacting the Anthem/CarelonRx at 1.833.727.2165. A pharmacy technician then works with your doctor to get the information needed for the review. Once Anthem/CarelonRx receives a completed prior authorization form from your doctor, they will conduct a detailed clinical review within three business days. Anthem/CarelonRx will then send you and your doctor notification regarding the prior authorization decision.
Specialty Pharmacy
If you are prescribed specialty drugs the Anthem’s Specialty Pharmacy, BioPlus, will be your specialty pharmacy. This specialty pharmacy partner will do more than just fill your prescriptions. You and your prescriber will be assigned a team to support you throughout the course of your specialty medication therapy.
To help you take full advantage of your enhanced specialty pharmacy program please note:
Whether your specialty medication is oral or injectable, or your caregiver, doctor, or you administer it, Anthem’s Specialty Pharmacy, BioPlus, can deliver your order to your physician’s office or to your home. Shipping is at no charge to you.
Your plan will cover up to a 30-day supply of your specialty medications at your plan’s copayment for a 30-day supply of specialty medications.
If you have questions, please contact Anthem/CarelonRx Customer Service at 1.833.727.2165
Summary of Benefits and Coverage
The Summary of Benefits and Coverage (SBC) document shows how you and the Archdiocese of Cincinnati Healthcare Plan share the cost of covered pharmacy services.
